 〉
診療・手術一覧
〉
Lymphedema treatment and surgery covered by insurance (one-day lymphatic venous anastomosis/LVA)
〉
診療・手術一覧
〉
Lymphedema treatment and surgery covered by insurance (one-day lymphatic venous anastomosis/LVA)
日本語ページはこちら
保険適用のリンパ浮腫の治療、手術について(リンパ管静脈吻合術)
If you are a distant patient or require urgent surgery due to the exacerbation of symptoms, we will make every effort to accommodate your needs by promptly adjusting the schedule.
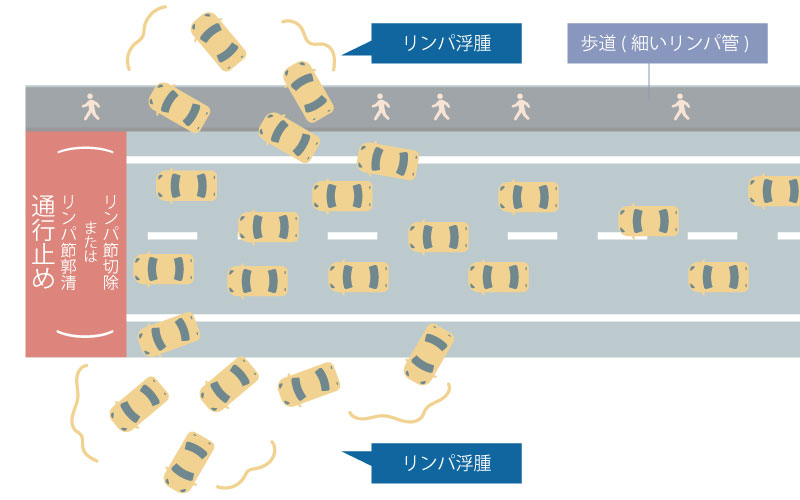
When the lymphatic vessels are compared to roads, lymph node dissection is similar to the "closure of the main road" as shown in the figures below.
 Effects of Lymphatic Depletion caused by Cancer
Effects of Lymphatic Depletion caused by Cancer
 After LVA surgery
After LVA surgery
Creating a lymphatic bypass is called microscopic lymphatic venous anastomosis (LVA), and performing it at the same time as cancer surgery is called prophylactic microscopic lymphatic venous anastomosis.
(Below, we present the latest papers that show the usefulness of prophylactic microscopic lymphatic vein anastomosis and give a short and simple explanation: Quotation from the Japanese Society of Clinical Oncology Lymphedema Clinical Practice Guidelines General Review)
Regarding the upper limbs, Boccardo et al. conducted a randomized controlled trial on the preventive effect of lymphedema by prophylactic lymphatic venous anastomosis after axillary dissection for breast cancer. They reported that the incidence rate of lymphedema in the prophylaxis group is quite low, and the volume increase of the affected limb in the prevention group was significantly less when comparing volumes before and after surgery (13).
Regarding the lower limbs, it has been reported that performing prophylactic lymphatic venous anastomosis near the dissected area during pelvic lymph node dissection for gynecologic malignancies effectively prevents the development of severe lymphedema, even during long-term follow-up periods of up to 13 years.
Prophylactic microscopic lymphatic venous anastomosis is not covered by insurance because it is performed as a preventive measure before the diagnosis of lymphedema. Additionally, since there are various methods of lymphatic drainage and lymphedema may not always occur, the procedure cannot be performed in all cases.
Therefore, “early diagnosis and early treatment” of lymphedema are considered to be important.
For early diagnosis,
1. Ultrasonography for lymphedema, 2. ICG lymphatic fluorescence test, 3. Photographing 4. Performing upper or lower limbs measurements.
The reason why early treatment is important is that the lymphatic transport function of the lymphatic vessels disappears depending on the degree or the time of lymphedema, and bypass surgery cannot be performed after the lymphatic vessels have lost their function.
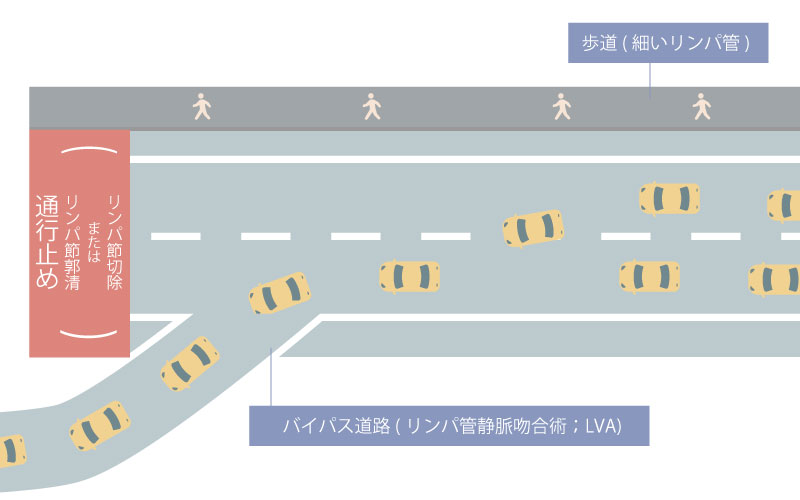
Our body is composed of approximately 60 to 70 percent water. Out of this, around 30 percent exists outside the cells and circulates throughout the body. The circulatory system is divided into two main systems: the hematological system, which includes the heart and the vascular system where blood flows, and the lymphatic system, through which lymph fluid flows in lymph vessels and lymph nodes.
The lymphatic vessels collect and transport excess extracellular fluid that cannot be taken up by capillaries, carrying it as lymph fluid. Eventually, this fluid is returned to the vascular system through the lymph nodes, helping to maintain a constant balance of extracellular fluid. This process is known as homeostasis.
In addition to its role in fluid balance, the lymph node also functions as an immune organ. Immune cells, such as lymphocytes, circulate within both the blood and lymphatic systems, serving as a defense mechanism against bacteria, viruses, and tumor cells.
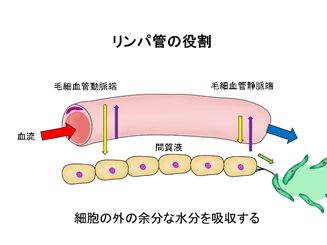
Lymphatic vessels are responsible for absorbing excess water outside the cells
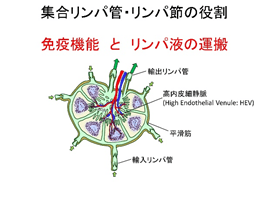
Aggregated lymph vessels and lymph nodes are responsible for immune function and lymphatic fluid transport
Lymphedema is a condition characterized by swelling of the arms and legs. It occurs when there is a disruption or reduced flow of lymphatic fluid, commonly as a result of treatment for breast cancer, uterine cancer, ovarian cancer, or malignant melanoma. Some individuals may also be born with the condition or develop lymphedema without a clear cause.
Lymphatic congestion or stagnation not only leads to swelling of the limbs but can also cause symptoms such as fatigue, warmth, and an increased risk of infection, known as cellulitis. This occurs due to the impaired function of the lymphatic system, including the lymph nodes. In the early stages of lymphedema, individuals may experience sensations of tightness, discomfort, or fatigue, even before visible swelling of the limbs occurs.
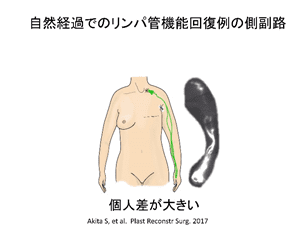
The onset of symptoms can vary from person to person, with some individuals experiencing symptoms shortly after cancer treatment, while others may develop symptoms years later. However, detailed imaging studies have indicated that many patients already show changes in their lymphatic flow within a year of undergoing cancer treatment[1] [2]。
The initial symptoms of lymphedema often manifest as non-visibly obvious signs, including tension, pain, heaviness, and fatigue. The way these symptoms are experienced can vary from person to person. While the feeling of swelling often subsides in the morning, it is often observed that lymphedema is already present upon examination.
Lymphatic fluid contains a significant amount of protein components. When the lymphatic vessels malfunction, causing these components to accumulate in the interstitial spaces outside the blood vessels in the subcutaneous tissue, an inflammatory reaction occurs. Additionally, since lymphatic flow plays a crucial role in immune response, compromised lymphatic flow also affects the normal immune response. Thus, lymphedema involves not only fluid accumulation but also progressive tissue hardening.
Post-cancer treatment lymphedema commonly occurs near the site where lymph node dissection or removal of the cancer was performed, such as the back and arms after breast cancer surgery, or the thighs, lower abdomen, and vulva after gynecological cancer surgery. In primary lymphedema, however, swelling is often experienced in the hands and feet. In some cases, swelling may begin in the hands and feet, particularly under the strong influence of anticancer drugs.
In developed countries like Japan, the most common cause of lymphedema is post-treatment for malignancy. However, primary lymphedema can also occur in the upper or lower extremities without a clear cause.
The severity of lymphedema is classified by the International Lymphatic Society as follows.
| Stage | Symptoms |
|---|---|
| 0 stage | A latent or asymptomatic condition in which lymphatic fluid transport is impaired but edema is not evident. Poor lymph flow, but no visible symptoms *ICG fluorescent lymphangiography shows that the initial changes have begun. |
| Stage I | Intertissue fluid with relatively high protein content is present, but it is still in the early stages and subsides with elevation of the extremity. Sometimes an indentation can be seen. Swelling has occurred, but it is in the early stage, so if you sleep with your legs or arms slightly elevated at night, you will feel refreshed in the morning.*ICG fluorescent lymphangiography shows clear reflux into the skin. |
| Stage II | Tissue swelling does not improve with elevation and indentation becomes evident. The lymphedema is in a gradual stage of progression, and irreversible tissue changes gradually develop. |
Late stage II | Tissue fibrosis is seen, and the indentations are no longer visible. This is advanced lymphedema, a stage in which significant changes in skin thickness and firmness have occurred. |
If lymphedema is left untreated, not only do the arms and legs gradually increase in size, but the skin also thickens, and the subcutaneous fatty tissue becomes firmer. If the condition is allowed to progress without treatment, it becomes increasingly challenging to restore it to normal.
Furthermore, since lymphatic vessels also function as pathways for immune cells, impaired lymphatic flow can easily lead to cellulitis. If left untreated and the condition worsens, cellulitis can cause skin fibrosis, resulting in a condition known as elephantiasis.
Cellulitis is an infection that affects the skin and subcutaneous fat layer. In lymphedema patients, cellulitis can cause a rapid onset of high fever and severe inflammation, often requiring emergency hospitalization. When cellulitis occurs, it further exacerbates the lymphedema itself by causing intense inflammation in the lymphatic vessels, making it more challenging to restore normalcy. Therefore, it is crucial to take necessary precautions to minimize the risk of cellulitis when managing lymphedema.
Elephantiasis is an advanced stage of lymphedema that occurs over a prolonged period. It is characterized by significant thickening of the skin, resembling an elephant's skin, and the hardening of subcutaneous tissue due to excessive fatty deposits and fibrosis. While images of elephantiasis found on the internet may cause concern, it is important to note that with proper care and early-stage treatment, the development of elephantiasis can be avoided.
A check that you can perform yourself is to measure the thickness of your arms and legs at the desired location.
Patients scheduled for treatments that carry a risk of lymphedema, such as cancer surgery or radiation therapy, are advised to measure the thickness of their arms and legs on both sides before undergoing treatment. Surprisingly, many patients initially have differences in the thickness of their left and right arms and legs.
Swelling in patients who have undergone lymph node removal surgery often begins near the site where the lymph nodes were located. For instance, in the case of breast cancer, it may occur in the arms and skin near the armpits, while in gynecologic cancer cases, it may appear in the thighs and lower abdomen. It is crucial to measure the thickness at the same location each time. For example, you can measure 10 cm above the crease of the bent elbow or at the location of a mole. Additionally, the thickness of the body can vary significantly between morning and evening. Therefore, it is important to compare measurements at the same time of day. If there is a notable difference throughout the day, it could indicate a compromised lymphatic system's ability to transport lymph.
The sensation of tension, pain, and heaviness can vary greatly from person to person, and many individuals report experiencing subjective symptoms in their arms and thighs even before visible swelling occurs. Early detection of lymphedema leads to more effective treatment. If you suspect something is wrong, we recommend seeking a consultation and examination with a medical specialist.
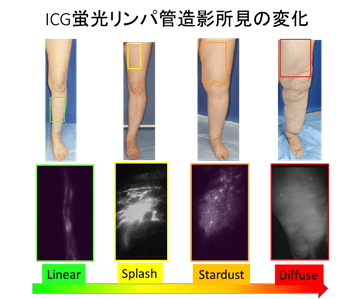
Although lymphoscintigraphy has long been considered the gold standard for diagnosing lymphedema, lymphatic function testing using indocyanine green (ICG) fluorescent lymphangiography has been reported to detect lymphatic abnormalities at an earlier stage.[3]
Furthermore, it is possible to assess whether the initial abnormalities observed in ICG indicate a high risk of developing chronic lymphedema since changes in ICG fluorescent lymphangiography findings can occur even before definite symptoms appear.[4]。
ICG fluorescent lymphangiography allows for a diagnosis to be made within an hour in the examination room. However, it is contraindicated for patients with iodine allergies. For those who cannot undergo ICG fluorescent lymphangiography, ultrasound can be used as an alternative to assess signs of lymphatic stasis by examining changes in lymph vessels and lymph nodes.[5]。

Lymphedema can be treated through conservative or surgical approaches. However, except for cases of very early lymphedema, a commitment to proper conservative treatment is a prerequisite before considering surgical treatment. It is crucial to understand the appropriate conservative treatment and daily care routine to maximize the benefits of surgical intervention.
The foundation of conservative treatment is complex physiotherapy, which encompasses four main components: skin care, medical lymphatic drainage, compression therapy, and exercise therapy tailored to individual symptoms.
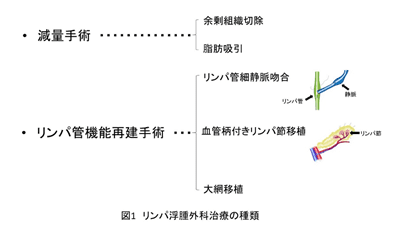
Surgical treatment for lymphedema can be categorized into functional reconstruction surgery, which aims to restore the function of lymphatic fluid transport, and weight loss surgery, which involves the removal of excess tissue. Functional reconstructive surgery is most effective in the early stages of the disease when there is still preserved function. In cases where the disease has progressed significantly and tissue degeneration is pronounced, a combination of functional reconstruction and weight loss surgery may be considered.
Functional reconstruction surgery can be broadly classified into two main procedures: lymphaticovenous anastomosis (LVA) and lymph node transplantation surgery.
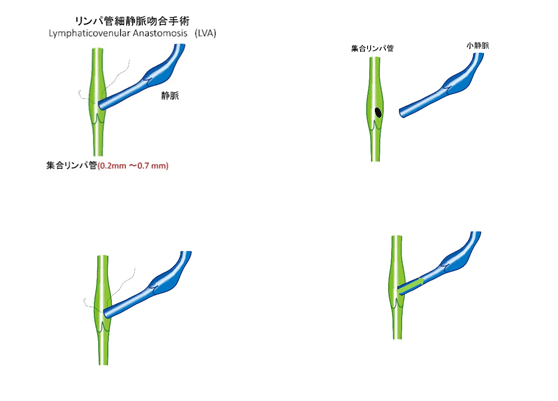
Method of anastomosing (stitching) lymph vessels and veins
Under local anesthesia, with the aide of a microscope, a lymphatic vessel with a diameter of around 0.5mm is anastomosed with a subcutaneous vein to create a path (bypass) for lymphatic fluid.
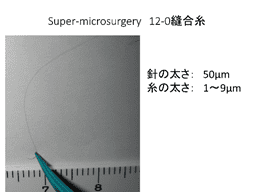
Needle thickness: 50μm
Thread thickness: 1-9μm
The surgery can be performed under a small amount of local anesthesia, so no special preoperative preparation is required. General anesthesia can be used if the patient is very uncomfortable with injectable anesthesia or if the patient experiences severe back pain, such as during long surgeries involving both lower limbs.
Immediately prior to surgery, ultrasound and ICG fluorescent lymphangiography are used to examine the location of lymphatic vessels and veins, determining the position of the skin incision. In areas with thin subcutaneous fat, a scar of less than 1 cm may be sufficient, but in areas with thick subcutaneous fat, a skin incision several centimeters in length may be necessary. Nevertheless, in most cases, the postoperative scar is not noticeable.
The bypass can be created by either a lateral end anastomosis, in which a horizontal hole is made in the lymphatic vessel and a thin vein is sewn into it, or an end anastomosis, in which the lymphatic vessel is cut and anastomosed with a thin vein. This depends on the relationship between the location and thickness of the lymphatic vessel and vein, and the flow rate of the lymph.
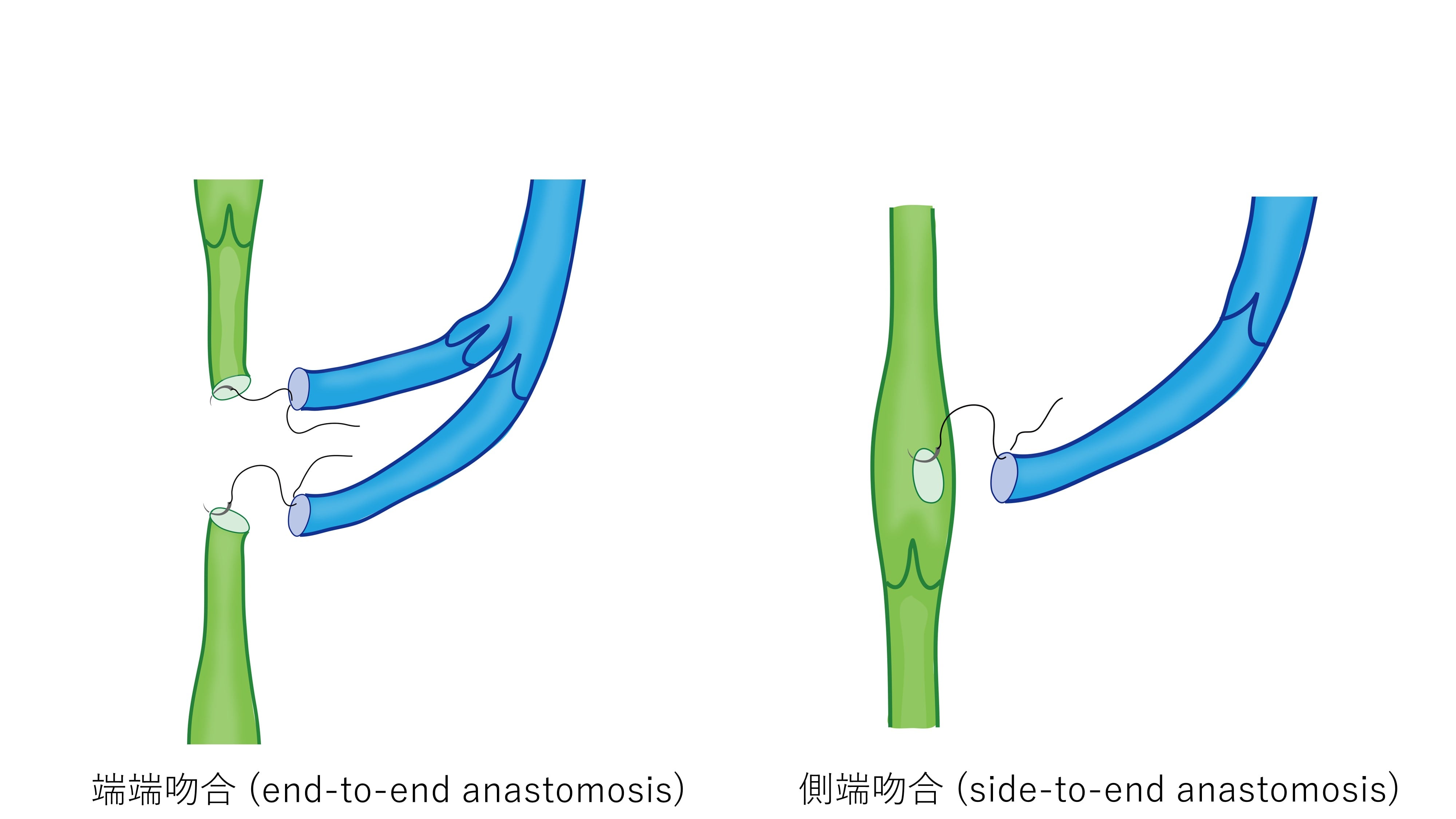
There are several types of anastomosis in which the lymphatic vessels and veins are sewn together. The two most common are end-to-end anastomosis, where the severed end of the lymphatic vessel is connected to the severed end of the vein, and side-to-end anastomosis, where a hole is created in the side of the lymphatic vessel and the vein is joined to this hole (see Figure 1).
Side-to-end anastomosis is commonly used in many medical facilities because it is easier to suture when the lymphatic vessels are thin. When two veins are present, it is recommended to connect both severed sections of the lymphatic vessel to the veins.
In a lateral anastomosis, since the lymphatic vessel itself is not cut, the original lymphatic flow is not obstructed in case of blockage in the connected area, and it also allows lymph flow to exit in the event of backflow through the vessel. However, this method can be challenging when the lymphatic vessels and veins are far apart or if the lymphatic vessels are very thin.
The surgeon has to be flexible to use either method based on the condition of the lymphatic vessels and veins.
Lymph node graft surgery involves transplanting a lymph node from a healthy site with normal lymphatic function to a swollen arm or leg. The feeding artery of the lymph node is then anastomosed with the graft site. This procedure is typically performed under general anesthesia and requires hospitalization, imposing a significant burden on the patient. However, due to its anticipated high therapeutic effect, it may be recommended depending on the results of imaging tests.
In advanced cases of lymphedema, liposuction, excision of subcutaneous tissue, or both may be performed. These procedures are carried out while ensuring that they do not obstruct the lymphatic flow. When combined with reconstruction of the lymphatic flow, a higher therapeutic effect can be expected.
| LVA手術(リンパ静脈管吻合術) | リンパ節移植術(LNT) | 脂肪吸引術(LS) | |
|---|---|---|---|
| 麻酔方法 | 局所麻酔 | 全身麻酔 | 全身麻酔または全身麻酔 |
| 手術時間 | 2〜3時間程度 | 5〜6時間程度 | 2〜3時間程度(吸引する範囲、切除する量による) |
| 手術の傷 | 1cm未満~2cm程度の切開が必要 | 小切開 | 小切開 |
| 術後のケア | 弾性ストッキング・弾性包帯による圧迫 | リンパ節採取部の圧迫 | 下肢全体の圧迫療法が生涯に渡り必要 |
| 身体的な負担 | 局所麻酔かつ日帰りのため極小 | 採取部の犠牲が伴うため侵襲性が大きい | リンパ管も吸引され破壊されるため侵襲性が大きい |
| 医療費の負担 | 保険適用・入院費用がかからない | 保険適用・7〜10日間の術後入院が必要 | 保険適用・2〜3日間の術後入院が必要 |
*Hospitalization
Lymphatic venous anastomosis (LVA) can be performed on an outpatient basis and does not require hospitalization. However, treatments involving general anesthesia may require hospitalization.
*Postoperative Precautions
If compression therapy was part of the preoperative treatment, it should be continued postoperatively at an equivalent level. Skin incisions will be protected with waterproof tape, and the skin will be sutured with both dermal and epidermal sutures. The stitches will need to be removed approximately 2 weeks after the surgery.
For successful surgical treatment of lymphedema, it is important to combine it with appropriate conservative treatment, except in the early stages. The surgeon performing the surgery should have knowledge of conservative treatment and be able to collaborate with facilities that provide conservative treatment.
Additionally, it is crucial to consult with a physician who is familiar with the various treatment options for lymphedema. Different surgical treatment options can be selected or combined based on the extent of lymphedema progression.
Weight gain not only leads to the accumulation of fat in the arms and legs but also negatively affects the lymphatic vessels' ability to transport lymphatic fluid. To reduce the risk of lymphedema and support the functioning of remaining lymphatic vessels in the case of lymphedema, it is important to pay attention to weight control.
Engaging in exercises that involve the muscles of the arms and legs helps facilitate the return of blood in the veins to the heart by utilizing the pumping action of the muscles. The smooth flow of blood in the veins is also crucial for proper lymphatic flow, as it influences the production of lymph fluid and the ease of flow where lymph vessels and veins intersect.
Moreover, since lymph vessels and lymph nodes play a significant role in the function of immune cells, it is important to consider that the immune system may be compromised in the arm or leg where lymph flow is obstructed, such as after lymph node removal surgery. Taking daily precautions to prevent the arm or leg from becoming a site of bacterial entry is essential, which includes refraining from scratching the operated area, wearing gloves when cleaning, and being attentive to conditions like athlete's foot.
At our clinic, our primary focus is on the treatment of lymphedema through lymphatic vessel anastomosis (LVA) using ultrasmall surgical techniques. The procedure is performed under local anesthesia, and we carefully connect lymphatic vessels and subcutaneous veins, typically around 0.5 mm in diameter, under a microscope to create a pathway or bypass for lymphatic fluid.
The effectiveness of the bypass relies on the pumping function of the lymph vessels and lymph nodes. By establishing the bypass early on using healthy lymph vessels, we aim to achieve a higher therapeutic effect.
In cases of upper extremity lymphedema, many patients no longer require compression therapy even in more advanced stages, whereas in the lower extremities, which are farther from the heart and subject to higher venous pressure, about 40% of very early lymphedema cases may no longer require compression. However, achieving the elimination of compression is more challenging in advanced lymphedema. [5] [6]。
Nevertheless, we have observed significant improvements in hand and foot thickness, reduced incidence of cellulitis (infection of subcutaneous tissue), and decreased compression pressure in advanced lymphedema cases.
In instances of advanced lymphedema, weight loss surgery such as liposuction may be combined with other treatments, or lymphatic tissue transplantation surgery may be considered. Prior to any surgical intervention, it is crucial to assess the patient's ability to comply with appropriate compression therapy, evaluate the presence of any vascular diseases, and engage in consultations to determine the appropriate treatment indications.
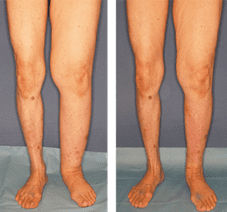
LVA case. Left - before surgery, Right - after surgery

LVA case. Left - before surgery, Right - after surgery
We perform day-of surgeries at our clinic and use local anesthesia.
お問い合わせ・ご予約はこちら
ご不明点や不安な点は
メールフォームからご相談ください。
〒104-0061 東京都中央区銀座2-8-19 FPG links GINZA 6F
Consultation and explanation of treatment and examination








* If CT, MRI, lymphoscintigraphy, etc. are required, patients would need to visit an affiliated medical institution.
It is recommended to have a follow-up examination approximately six months after the surgery to evaluate the status of lymphatic flow and assess the progress of the treatment.
We recommend that you continue the same compression therapy before surgery until the postoperative examination.
*For patients who reside far from our clinic, we will introduce affiliated facilities nationwide.
Our clinic treats many patients with lymphedema following treatment for malignant tumors (cancer). Once lymphedema develops, there is a lifelong risk of disease progression, so it is recommended to start treatment as early as possible. On the other hand, patients are often physically weak immediately after treatment for malignant tumors, and adjuvant therapy is often a priority.
Since one day lymphatic venous anastomosis is a minimally invasive procedure, treatment during hormonal therapy for breast cancer is not a problem. It can sometimes be performed between treatments if the patient is undergoing anticancer therapy with infrequent white blood cell depletion with the patient doctor's permission. If you wish to see us before the completion of adjuvant therapy for malignant tumors, we recommend that you consult with your primary doctor and ask to prepare a referral letter for you to collaborate with our clinic
Lymphatic venous anastomosis (LVA) is a highly advanced and skilled procedure that can only be performed by a doctor who has the expertise to connect blood vessels and lymphatic vessels less than 0.5 mm in diameter, in the field of supermicrosurgery (ultra-microsurgery).
If performed by an inexperienced physician, the lymphatic vessels can be damaged, leading to the leakage of lymphatic fluid and accelerating the progression of lymphedema.
Lymphedema can also worsen over time and may be influenced by factors such as age and weight changes. Therefore, we recommend working with a physician who will provide ongoing treatment and long term support.
Although complications such as lymphatic fluid leakage through the incision site or visible scarring may occur, these complications are extremely rare due to the extensive experience of our doctors, who have been performing lymphatic venous anastomosis (LVA) for many years.
Chiba University Plastic Surgery Lecturer
Akita Shinsuke
Lymphedema is a common condition that can occur after surgery for breast cancer and gynecological malignancies. However, it can also have other causes, including primary lymphedema, which has no clear trigger. In recent years, the development of techniques such as lymphatic vein anastomosis, lymphatic tissue transplantation, and liposuction has significantly improved the outcomes of surgical treatment for lymphedema.
Nevertheless, there is a lack of standardization in the diagnosis and treatment of lymphedema, and many patients may be struggling with the condition without proper guidance. We encourage you to contact us for a consultation to discuss your specific situation and explore potential treatment options.
All medical care will be covered by insurance.
*The high-cost medical care benefit system can be applied to surgery.
| Medical certificate | US$200/page |
|---|
(tax included)
 LVA手術とはどのような手術ですか?
LVA手術とはどのような手術ですか?
リンパ管静脈吻合術といって、下肢や上肢でリンパ管と静脈のバイパスを作り、新たなリンパ管の流れを作る手術です。局所麻酔をし、顕微鏡を覗きながら直径0.5mm前後のリンパ管と皮下静脈を吻合し(つなぎ合わせ)ます。
 LVA手術にはどのくらい費用がかかりますか?
LVA手術にはどのくらい費用がかかりますか?
手術費用は健康保険の対象となります。また、高額療養費制度の適用があります。民間の医療保険の対象もなります。
 LVA手術での入院期間はどれくらいですか?
LVA手術での入院期間はどれくらいですか?
大学病院などでは入院で行われることもありますが、銀座リプロ外科では日帰りの手術が可能です。
 なぜ日帰り手術が可能なのですか?
なぜ日帰り手術が可能なのですか?
低侵襲で体への負担が少なく、小切開で痛みの少ない局所麻酔で手術を行うことができます。術直後から水分や食事の経口摂取、歩行などが可能です。
 LVA手術の傷跡は残りますか?
LVA手術の傷跡は残りますか?
皮下脂肪の厚さによって1cm未満~2cm程度の切開が必要です。体質にもよりますが、傷跡はほとんどの場合とても薄くなり、気になるほどの傷跡にはなりません。
 手術後も治療は続けなくてはなりませんか?
手術後も治療は続けなくてはなりませんか?
術後に症状改善がみられても、再び症状が出るリスクを軽減するため、原則として弾性着衣による圧迫療法は継続して行ってください。
当院では、術後のケアや弾性着衣の履き方など、なんでもご相談いただけるリンパルームを併設しています。お気軽にご利用ください(完全予約制)
 自分のリンパ浮腫の状態にあった治療方法がわかりません
自分のリンパ浮腫の状態にあった治療方法がわかりません
リンパ浮腫は、早期発見・早期治療で進行を抑え、症状を軽減することが可能です。
がんの手術場所によって発症しやすい場所がある程度決まっているので、日ごろからむくみがないか確認し、違和感があればなるべく早く受診し、専門医と治療方法を相談しましょう。
[1] Akita S, Mitsukawa N, et al. Early diagnosis and risk factors for lymphedema following lymph node dissection for gynecologic cancer. Plast Reconstr Surg. 2013; 131: 283-90.
[2] Akita S, Nakamura R, et al. Early Detection of Lymphatic Disorder and Treatment for Lymphedema following Breast Cancer. Plast Reconstr Surg. 2016; 138: 192e-202e.
Lymphedema was often diagnosed after a significant period of time. However, in a cohort study that utilized ICG fluorescence lymphangiography to assess lymphatic function periodically within one year after lymphadenectomy for gynecologic malignancies or breast cancer surgery, the emergence of chronic lymphedema findings on imaging studies was observed in many cases. These imaging changes were detected before any noticeable change in limb circumference, typically at the time when patients experienced symptoms such as limb tension, pain, or paresthesia.
[3] Akita S, Mitsukawa N, Kazama T, Kuriyama M, Kubota Y, Omori N, Koizumi T, Kosaka K, Uno T, Satoh K.
Comparison of lymphoscintigraphy and indocyanine green lymphography for the diagnosis of extremity lymphoedema.
J Plast Reconstr Aesthet Surg. 2013: 792-8.
An imaging test called lymphoscintigraphy has been used as the gold standard to identify early-stage lymphedem. However, it is performed at hospitals equipped with RI (radioisotope) facilities which exposes patients to radiation. Lymphoedema severity by ICG fluorescence lymphangiography correlated strongly with scintigraphic severity, and ICG fluorescence lymphangiography has been shown to be superior in its ability to detect early changes associated with lymphedema.
[4] Akita S, Mitsukawa N, et al. Suitable therapy options for sub-clinical and early-stage lymphoedema patients. J Plast Reconstr Aesthet Surg. 2014; 67: 520-5
In patients who have undergone lymphadenectomy for gynecologic malignancies, ICG fluorescence lymphangiography showed a very early change (splash pattern) before clinical symptoms appeared. It has been observed that individuals with this pattern have a 1.62 times higher likelihood of developing chronic lymphedema compared to those without it.
The emergence of a "stardust pattern" on ICG fluorescence lymphangiography indicates the development of chronic lymphedema. It has been reported that forlower limbs lymphedema, if lymphatic anastomosis is performed in the early stage when the stardust pattern appears, 44.8% of patients do not need compression treatment.
[5] Akita S, Yamaji Y, et al. Intraoperative Detection of Efferent Lymphatic Vessels Emerging from Lymph Node during Lymphatic Microsurgery. J Reconstr Microsurg. 2019; 35: 372-378.
ICG fluorescence lymphangiography is a minimally invasive examination method; however, it can cause slight discomfort because it involves an injection. It should be noted that individuals with an iodine allergy cannot undergo this specific examination.In cases of lower limb lymphedema, studies have reported that changes in the size of lymph nodes at the base of the foot (inguinal region) and the thickness of lymphatic vessels draining from those nodes can be detected during the early stages of ICG fluorescence lymphangiography. If an ICG test is not feasible or if there are concerns about it, an alternative option is to undergo an ultrasound examination. Ultrasound can provide valuable information and assist in the assessment of lymphedema.
[6] Akita S, Mitsukawa N, et al. Comparison of vascularized supraclavicular lymph node transfer and lymphaticovenular anastomosis for advanced stage lower extremity lymphedema. Ann Plast Surg. 2015; 74: 573-9.
In advanced stages of lymphedema, lymphaticovenular anastomosis (LVA) can be performed to reduce limb thickness and decrease the frequency of cellulitis. LVA is considered an excellent treatment option as it has fewer complications compared to other surgical treatments such as lymph node transplantation. However, it is exceptionally rare to completely eliminate the need for compression therapy in advanced lymphedema cases. In the management of advanced lymphedema, it is crucial to establish an optimal care approach by combining LVA with appropriate compression therapy.
c 2019 Association of Microsurgery, Ginza Reproductive Surgery.