
このページの監修医師
Varicocele is a condition in which varicose veins (dilation of veins) are found in the testis and the sperm (three-layered membrane that covers the vas deferens, vascular nerves, nerves, and lymph vessels). It is found in 15% of general males and is suspected in 40% of male infertility patients. Here, we introduce the causes and adverse effects of varicocele. In addition, we will also introduce surgical methods and preventive methods.

このページの監修医師

日本語ページはこちら
精索静脈瘤
Varicose veins (dilation of veins) are found in the testicles and the spermatic cord above it, and this is called a varicocele.
Varicocele is found in 15% of general men, in more than 40% of male infertility patients, and is responsible for 78% of acquired male infertility (second infertility).
According to the WHO report, a survey of 9,034 infertile men found varicocele in 25.6% of men with poor semen findings and 11.7% of men with normal semen findings.
First, we will perform an examination and judge the indication for surgery on the condition of semen findings and palpation.
There are upper microsurgical ligation, standard lower ligation, and one-day lower microsurgical ligation.
Upper microsurgical ligation and one-day lower microsurgical ligation are commonly performed.
At our clinic, we perform a one-day lower microsurgical ligation Nagao method at your own expense.
>> Please refer to the special page for surgery
In varicoceles, retrograde blood flows through veins in the testicles. This results in blood congestion around the testes. 15% of men develop varicoceles, and it is estimated that 40% of infertile men develop this symptom. Testicular varicoceles may cause deterioration of testicular function, testicular atrophy, semen deterioration, damage to sperm DNA, scrotal pain and discomfort, and a decrease in male hormone levels. Although sometimes asymptomatic, varicoceles are typically associated with unevenness of the scrotum, swelling, and pain. If varicocele is found, significant improvement in semen findings can be expected * 1. If you have a semen test at another hospital and have been diagnosed with bad findings, we recommend that you have a checkup.
* 1 From the European Urology Society: Male Infertility Practice Guidelines
The regurgitation of blood from the veins of the kidneys causes congestion of the upper scrotum in the left testicular vein, resulting in symptoms such as hump-like swelling.
This causes blood to stagnate and the temperature of the testicles to rise. And it causes the testicular function to deteriorate.
Click here for more information on male infertility
In many cases, there are no subjective symptoms. However, when it gets worse, bumps, pain in the scrotum, and swelling of the scrotum appear.
Varicocele has the following effects:
In the case of mild symptoms, surgery is not necessary, but at our clinic, "Grade 3 (visible: the testicles are uneven, swollen)" and "Grade 2 (touchable: swollen)" ”, Surgery is indicated for veins with a thickness of 3 mm or more around the testis or multiple veins of 2.8 mm or more in ultrasound.
Varicocele may be severely painful or painless. Even if you feel dull pain occasionally at first, as it progresses, it becomes more frequent and the degree of pain changes to sharp pain.
In addition, there are many people who are painless, have delayed detection of varicocele, and become male infertile when they notice it.
Besides that, varicocele is more likely to cause inflammation of the epididymis. Epididymitis is treated with analgesics, anti-inflammatory drugs, and in some cases antibacterial agents, but once it is done, inflammation will occur repeatedly unless treatment for varicocele is treated.
(Some people who have been seen in the urology department have been diagnosed with prostatitis and are prescribed medicine for it, but it is necessary to distinguish between epididymitis and prostatitis.)
It is stated in the guidelines of the world including Europe and the United States that it is deeply related to male infertility.
The testicles function when the temperature of the testicles is 2-3 degrees lower than the body temperature. If the varicocele is left untreated, testicular function (the ability to make sperm and androgens) deteriorates.
As mentioned at the beginning, varicocele is found in 15% of general males, in more than 40% of male infertility patients, and is responsible for 78% of acquired male infertility (second infertility).
According to a WHO report, a survey of 9034 infertile men found varicocele in 25.6% of men with poor semen findings of 11.7% compared to men with normal semen findings.
It is important for men as well as women to treat infertility.
Originally, venous blood returning from the testicles to the heart
For these reasons, refluxed venous blood accumulates around the testes and causes varicocele.
There is no heredity or specific cause, but bipedal humans tend to have poorer blood return from below the heart than quadrupedal animals.
Varicose veins on one side also adversely affect the testicles on the other.
It is not a rare disease, with 15% of general men and 40% of infertile men.
There is no heredity or specific cause for the regurgitation of venous blood.
Blood is carried from the heart through arteries to the whole body, and from the whole body through veins to the heart. Arterial flow is created by the beating of the heart. On the other hand, the flow of veins is created by gravity, muscle movement, and venous valves from above the heart. Below the heart, muscular movements and venous valves alone return blood to the heart against gravity. If the muscles and venous valves are weak, the ability to return blood to the heart is impaired, causing blood reflux and varicose veins.
In addition, blood returns from the varicocele to the left renal vein, but in varicocele, a nut cracker phenomenon occurs in which the left renal vein is pressed against the abdominal aorta and superior mesenteric artery, resulting in poor blood return.
Varicocele is examined by "palpation" and "ultrasound".
By palpation, it is classified into grades 1 to 3 according to the degree of varicose veins. At our clinic, surgery is indicated for grade 2 or higher.
| Grade | symptom |
|---|---|
| Grade 1 | Can be checked by touching while standing and under abdominal pressure load |
| Grade 2 | Touch while standing and see swelling |
| Grade 3 | You can see that the scrotum is uneven and swollen |
In addition, ultrasound confirms the thickness of veins around the testes, and if either "multiple thicknesses of 3 mm or more" or "many of them have a thickness of 2.8 mm or more", surgery is applied.
Treatment is done by surgery. There are multiple surgical methods, and it is necessary to consider the risk of complications and the recurrence rate. We recommend "One-day microscopic varicocele low-level ligation / Nagao method".
The table below summarizes the surgical procedures for varicocele by feature.
References
1. European Urology Society Male Infertility Guidelines
2. K. Nagao: One day microsurgical varicocelectomy under local anesthesia.
IFFS / JSRM International Meeting (Symposium), Yokohama, 2015
* In Japan, the recurrence rate is the same as that of inguinal ligation because the external varicocele is left.
The features of each operation are introduced below.
Laparoscopic surgery is generally referred to as "minimally invasive surgery (surgical method with less effect on the body)", but it is necessary to always fill the abdominal cavity with carbon dioxide during surgery, and the surgery is performed in a position where your head is facing down. Because of the lowered posture, it actually puts a strain on the body. In addition, it is said that it is difficult to deal with bleeding.
Percutaneous embolization puts an embolic material into a vein, so it's okay when you're standing and regurgitating, but it can cause blood to reach your heart when you sleep. Then, the embolic substance goes through the heart to the cerebral blood vessels and cardiovascular blood vessels.
Laparoscopic surgery and percutaneous embolization are also characterized by high complications and recurrence rates. Especially in percutaneous embolization, multiple small veins cannot be embolized (blocking blood vessels), and the bypass blood vessels dilate immediately, resulting in a high recurrence rate.
Lymphatic vessels cannot be preserved by macroscopic high-level ligation. Therefore, the complication rate of testicular edema is high, and the recurrence rate is also high because the external sperm (reflux) vein remains.
In high-level ligation under a microscope, the lymphatic vessels are preserved and there is no complication of testicular edema, but the recurrence rate is 5% because the external sperm (reflux) vein remains.
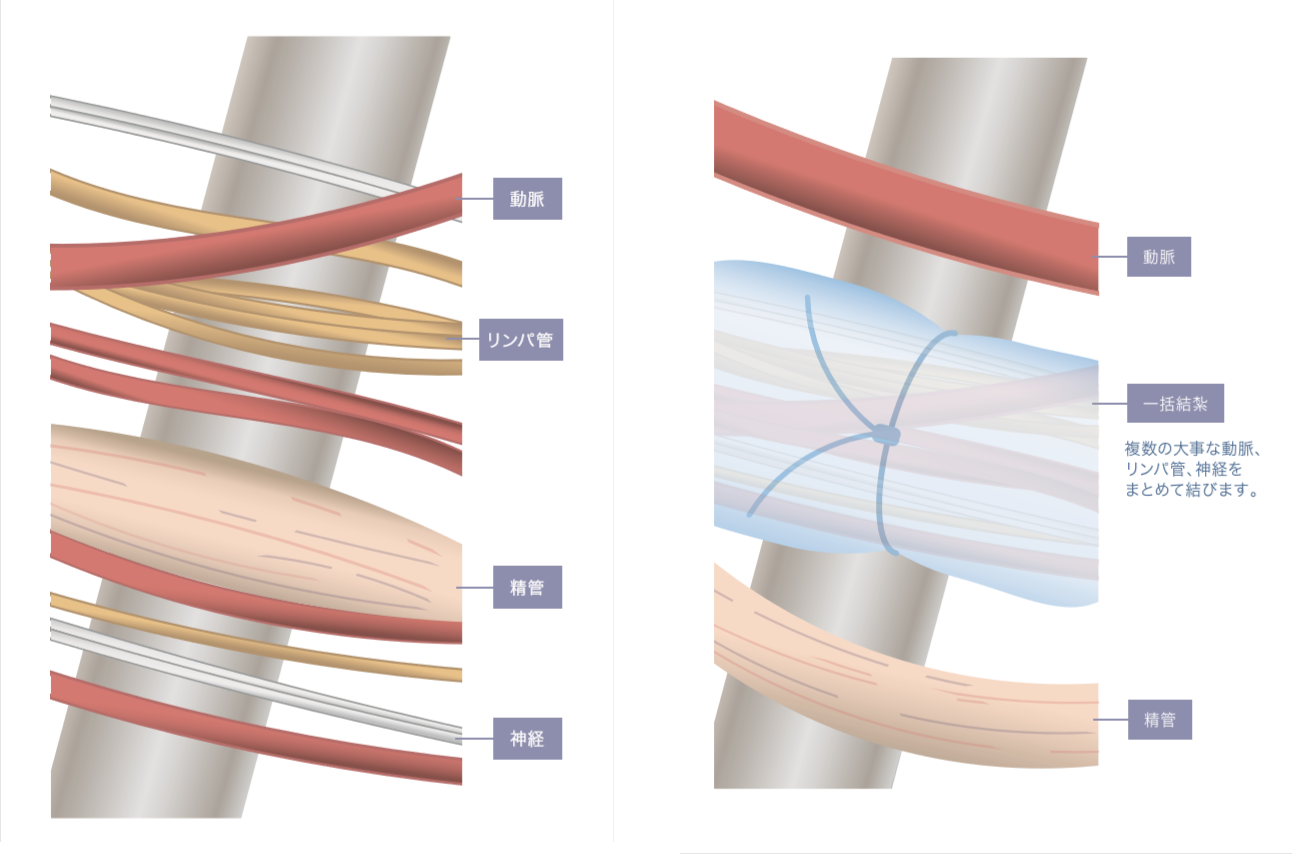
In addition, general microscopic low-level ligation involves damage to multiple arteries, lymph vessels, and nerves, which can lead to serious complications such as testicular edema, poor blood flow, and testicular atrophy.
In addition, the recurrence rate is high because the external sperm (reflux) vein remains.
In this way, past surgical procedures had a high recurrence rate and the possibility of complications remained, so it was not always the best choice.
Therefore, we recommend the advanced technique "day-trip microscopic varicocele low-level ligation / Nagao method" developed by Professor Koichi Nagao, director of the Reproduction Center, Toho University Omori Hospital.
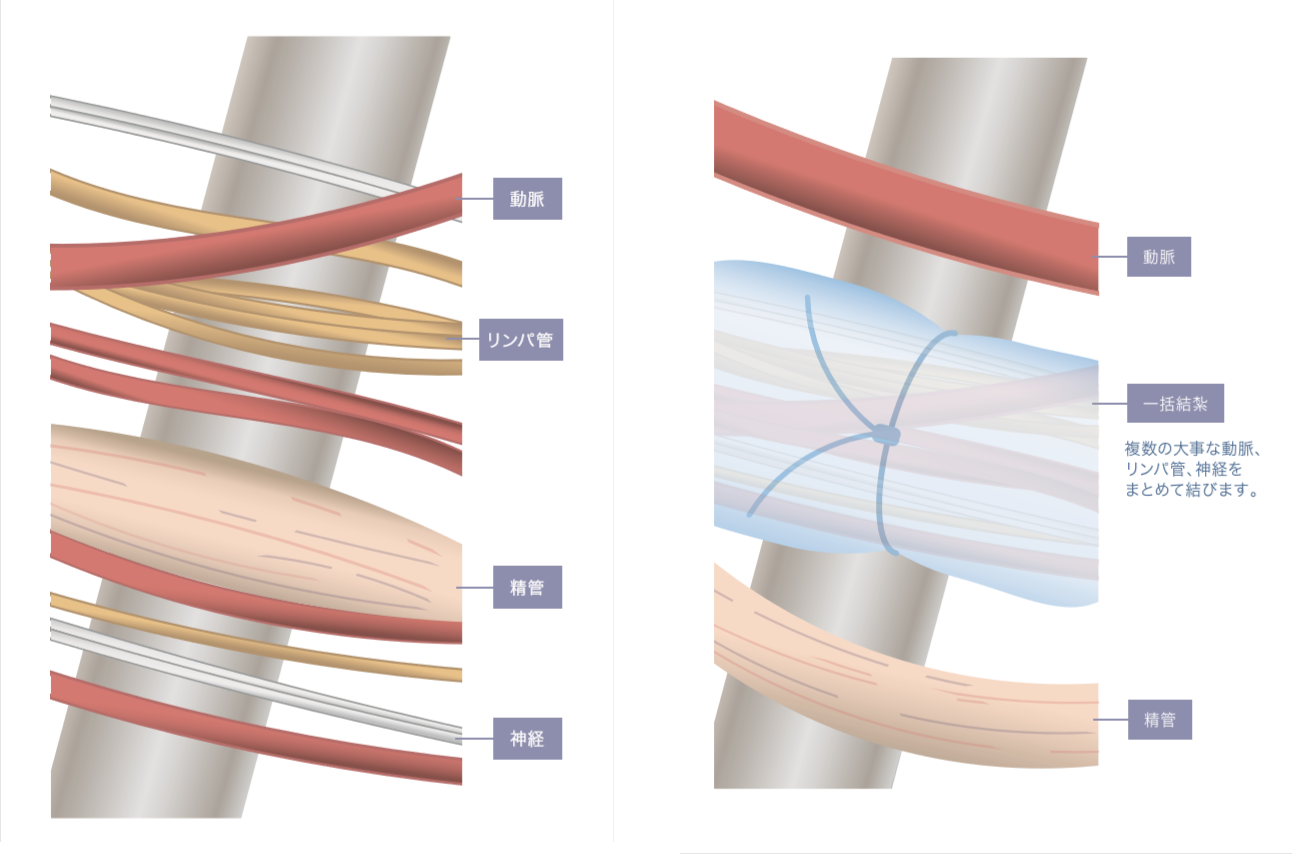
In the one-day varicocele low-level ligation / Nagao method, a highly skilled surgeon separates blood vessels (arteries / veins), lymph vessels, and nerves one by one. As a result, everything important is preserved and there are rarely any complications. It also reliably ligates the external sperm (reflux) vein and other regurgitation veins, resulting in a recurrence rate of 0.1%, the lowest compared to other surgical procedures.
Click here for more information on Nagao Method Surgery
(tax included)
Currently, no suitable method has been found to prevent varicocele. However, it is possible to improve reproductive function by finding it early and performing appropriate surgery.
Therefore, do a self-examination and aim for early detection. Also, if you have any concerns, please consult your doctor immediately.
Click here for details on surgery
・Azoospermia
Azoospermia is roughly classified into the following two types.
・Obstructive azoospermia
・Non-obstructive azoospermia
Obstructive azoospermia is a condition in which sperm are produced in the testicles but the vas deferens are blocked and do not come out. If treatment is possible, sperm reconstruction is performed, and if reconstruction is not possible, intratesticular sperm collection is performed under a microscope, followed by microinsemination.
Non-obstructive azoospermia is a condition in which sperm is not produced in the testicles. There are various causes, but the first is a blood test for hormones. If there are no abnormalities as a result, intratesticular sperm collection is performed under a microscope, and if sperm are found, microinsemination is possible.
In addition, if it is deemed necessary as a result of the hormone test, a chromosome test (G band method) and a Y chromosome microdeletion (AZF) test will be performed. If there is a chromosomal abnormality or a deletion on the Y chromosome, it cannot be treated.
・Oligospermia and asthenozoospermia
Oligospermia is a condition in which there are few sperms in the semen, whereas asthenozoospermia is a condition in which mental motility is poor, and both may occur together.
If you have a varicocele, surgery can help improve your semen. If you do not have varicocele, we recommend medical coenzyme Q10 100 mg (daily) or clomiphene 25-50 mg (daily).
・ Erectile dysfunction
There are many cases of ED due to the timing method of fertility treatment. In that case, ED treatment will improve it. In addition, there are many people with vaginal ejaculation disorders who cannot ejaculate in the vagina even if they can ejaculate by masturbation. In such cases, you can remove the penis once during sexual intercourse, ejaculate in a cup, and then inject semen into the vagina with a syringe (without a needle).
Gynecological treatment is determined by the semen findings of men, so it is recommended that you check with your husband for varicocele before proceeding.
Varicocele accounts for 40% of male infertility and is the only treatable disease.
Varicocele damages sperm genes (DNA and chromosomes) and makes semen worse. Treatment increases pregnancy and childbirth rates and reduces the risk of miscarriage and malformations in all methods of microinsemination, artificial insemination, in vitro fertilization, and natural (timing).
Also, treatments given in gynecological treatment do not improve male reproductive function. Intratesticular sperm extraction (TESE) is a surgical procedure that reduces reproductive function. Adjuvant therapies and lifestyle changes may be effective, but the medical basis is not high.
Varicocele can be easily diagnosed by palpation and ultrasound. Before considering gynecological treatment, be sure to have a varicocele test.
Learn more about male infertility
 What is Varicocele?
What is Varicocele?
Varicocele is a disease in which varicose veins (dilation of veins) occur in the testicles and the spermatic cord above them. It is found in 15% of general men, and it is said that more than 40% of male infertility patients are infertile due to varicocele. Surgery is used for treatment.
 Is varicocele surgery covered by insurance?
Is varicocele surgery covered by insurance?
It depends on the surgery. In the case of surgery covered by insurance, even if the medical expenses are 400,000 to 600,000 yen (in the case of 30% burden), the self-pay is 140,000 to 170,000 yen. However, there is a risk of complications in the surgical procedure covered by insurance, so we recommend one-day microscopic varicocele low-level ligation (Nagao method), which is an operation not covered by insurance.
 Is there a cause of varicocele?
Is there a cause of varicocele?
When blood flows back from the kidneys to the veins around the testicles, the veins dilate into the testicles and spermatic cord. This is the cause of varicocele. It is said that varicocele causes 35% of oligospermia and decreased sperm motility, which are known to cause male infertility.
 Is there pain for varicocele?
Is there pain for varicocele?
Varicocele may be severely painful or painless. Even if you feel dull pain occasionally at first, as it progresses, it becomes more frequent and the degree of pain changes to sharp pain.
Varicocele is also prone to epididymitis, which can be painful.
In addition, there are many people who are painless, have delayed detection of varicocele, and become male infertile when they notice it. If you feel pain, please contact us from here.
 What happens if I leave it without surgery?
What happens if I leave it without surgery?
Varicocele reduces testicular function, deteriorate semen, testicular atrophy, and androgens. In addition, pain such as scrotum may also appear.
Deterioration of semen damages sperm genes (chromosomes and DNA), leading to future male infertility. When the amount of male hormones is low, it leads to early male menopause, which also causes a decrease in motivation.
Poor testicular function also poses a risk of testicular calcification and testicular cancer.
〒104-0061 東京都中央区銀座2-8-19 FPG links GINZA 6F

永尾 光一 先生
東邦大学 医学部教授(泌尿器科学講座)
東邦大学医療センター大森病院 リプロダクションセンター
東邦大学医療センター大森病院 尿路再建(泌尿器科・形成外科)センター長
昭和大学にて形成外科学を8年間専攻。その後、東邦大学で泌尿器科学を専攻し、形成外科・泌尿器科両方の診療科部長を経験する(2つの基本領域専門医を取得)。得意分野はマイクロサージャリーをはじめとする生殖医学領域の形成外科的手術。泌尿器科医の枠を超えた細やかな手術手技と丁寧な診察で、様々な悩みを抱える患者さんから高い信頼と評価を得ている。
所属医療機関
〒104-0061 東京都中央区銀座2-8-19 FPG links GINZA 6F